Anthrax, a disease often associated with livestock and rural exposure, has resurfaced in Zimbabwe with over 135 confirmed cases reported as at October 12, 2025, according to the Ministry of Health and Child Care’s Weekly Disease Surveillance Report.
While no fatalities have been recorded, the outbreak has re-ignited concerns about public awareness, veterinary control and rural health infrastructure.
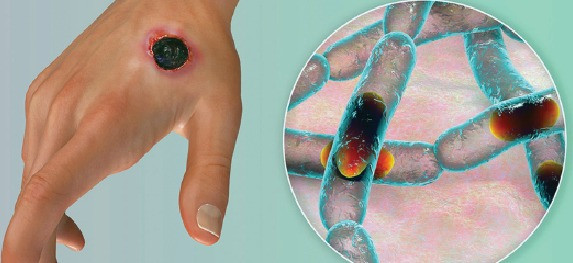
Anthrax is a rare but serious infection caused by the bacterium bacillus anthracis. It mainly affects animals such as cows, sheep and goats, but can spread to humans through contact with infected animals or contaminated animal products. The illness takes different forms depending on how the bacteria enters the body.
Causes
Cimas Health Group doctor Bekezela Ndhlovu emphasised the importance of understanding the disease’s transmission and symptoms.
“The way anthrax enters the body determines how it makes you sick. When anthrax spores enter through a cut or scrape on the skin, they cause a raised itchy sore that develops into a black-centred ulcer. If inhaled, the spores can lead to severe respiratory illness, beginning with flu-like symptoms and quickly progressing to breathing problems and shock,” Ndhlovu said.
“Eating contaminated meat can cause nausea, vomiting and abdominal pain. Though potentially deadly, anthrax can be treated effectively with antibiotics if detected early, and vaccines are available for people at higher risk.”
In Zimbabwe, the disease is most commonly transmitted through the consumption of contaminated meat and contact with infected cattle, particularly in rural settings.
- Building narratives: Chindiya empowers girls through sports
- Building narratives: Chindiya empowers girls through sports
- Nama successfully hosts second golf day
- Nama successfully hosts second golf day
Keep Reading
“In rural parts of Zimbabwe, anthrax is most transmitted to humans through the consumption of contaminated meat and may be transmitted also through contact with infected cattle.
“People can become infected when handling, slaughtering, or skinning animals that are sick or have died from anthrax. In many cases, the meat comes from uninspected animals or from cattle that have died suddenly, often without clear cause,” he explained.
Symptoms
The disease manifests in three primary forms: cutaneous, gastrointestinal and inhalation anthrax, with each presenting distinct clinical symptoms and risks.
“Cutaneous (skin) anthrax is the most common form of anthrax. It begins as a small, itchy bump that resembles an insect bite and soon develops into a painless sore with a black centre. Other symptoms may include fever, headache, muscle aches and vomiting. With prompt treatment, recovery is likely.
“Gastrointestinal anthrax occurs after eating contaminated meat from infected animals. It usually starts with nausea, loss of appetite, vomiting, and abdominal pain, followed by severe diarrhoea. In advanced cases, patients may vomit blood and experience intense abdominal pain,” Ndhlovu said.
“Inhalation (pulmonary) anthrax is the most dangerous form of the disease. It begins with mild, flu-like symptoms such as fever, sore throat, and fatigue. As it progresses, it can cause severe breathing difficulties, chest pain, and shock. Without early treatment, this form is often fatal,” he added.
Response
The Health ministry has responded to the outbreak with heightened surveillance and public health messaging, but challenges remain. Rural communities, where livestock is central to both diet and income, are particularly vulnerable.
“Certain communities and occupations in Zimbabwe face a higher risk of anthrax infection. People who work closely with animals are the most vulnerable. This includes veterinarians, farmers and abattoir workers who handle, slaughter or dress livestock and game meat. Laboratory staff who work with anthrax samples are also at risk if proper safety measures are not followed,” Ndhlovu said.
He added that people living in areas known as anthrax hotspots, where outbreaks have occurred in the past, face increased exposure. These communities are often rural and rely heavily on livestock for their livelihood, making them more likely to come into contact with infected animals or contaminated meat.
“The early symptoms of anthrax depend on how the infection enters the body and they can appear anywhere from one day to two months after exposure. Recognising these warning signs early is key to getting life-saving treatment.”
Diagnosis
He went on to say in terms of diagnostics, Zimbabwe’s approach is largely clinical.
“In Zimbabwe it is not generally recommended to take a laboratory specimen, cases are to be treated on a clinical and epidemiological basis. This means individuals presenting with the typical symptoms and history and form places where there is an outbreak, are to be treated based on a clinical diagnosis.
“Anthrax is, and can however, be confirmed through laboratory testing, as its symptoms can resemble other common illnesses. A blood sample or a biopsy from a skin sore (ulcer) can be taken to look for the bacillus anthracis bacteria under a microscope or through culture tests.
“In more severe cases, especially when anthrax is suspected to have spread through inhalation or to the brain, additional tests such as a lumbar puncture (to test spinal fluid) or use imaging tools like a chest X-ray or CT scan to detect signs of infection in the lungs,” he said.
The information in this article is provided as a public service by the Cimas iGo Wellness programme, which is designed to promote good health. It is provided for general information only and should not be construed as medical advice. Readers should consult their doctor or clinic on any matter related to their health or the treatment of any health problem. — [email protected] or WhatsApp 0772 161 829 or phone 024-2 773 0663.