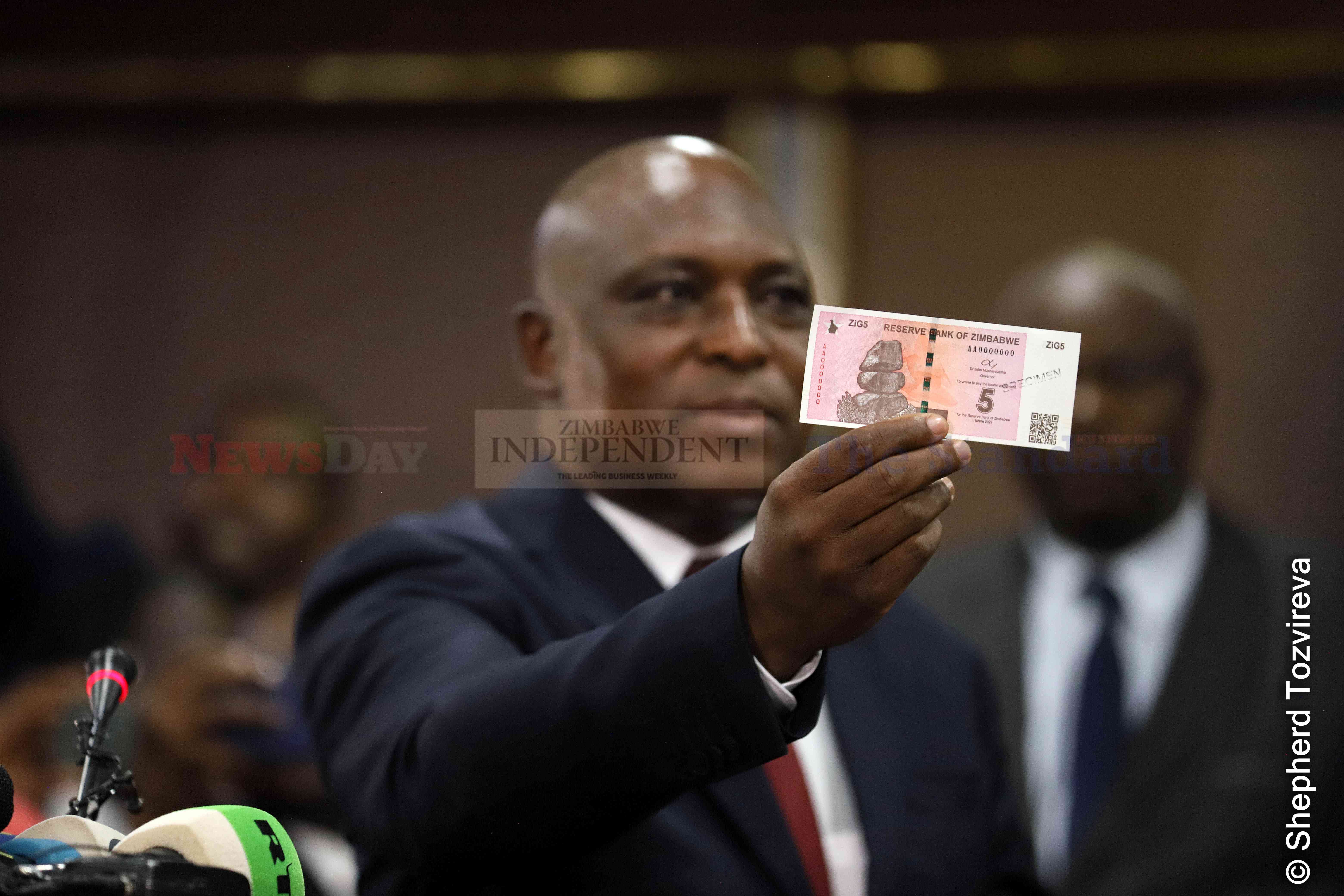
The ZiG was introduced following the rapid depreciation of the Zimbabwe dollar (ZWL).
‘New currency averted systems crash’

It replaced the Zimbabwe dollar (ZWL), which had to be decommissioned after depreciating rapidly against the US dollar, complicating an already dire economic situation.
Advisory sees hefty spinoffs in RTG deal
By Shame Makoshori
Apr. 19, 2024
Telecoms note sharp investment decline
Business Digest
By Melody Chikono | Apr. 19, 2024
‘Inflation forecast unrealistic’
As such, monthly inflation rates are expected to be well below 1%, while annual inflation is projected to close the year below 5%.
By Mthandazo Nyoni
Apr. 19, 2024
Fair game in Zim, China trade
By Julia Ndlela
Apr. 19, 2024
Rest, good sleep contribute to better health, happiness
By Admin
Feb. 17, 2023
Everyone eligible is encouraged to donate blood, help save lives
By The Independent
Jun. 10, 2022
Cottco sets aside US$3,5m for new projects
By Blessed Ndlovu
Apr. 19, 2024
Nissan dealership targets to grow sales by 15%
By Tatira Zwinoira
Apr. 19, 2024
Review of the 2024 Monetary Policy Statement
By Prosper Chitambara
Apr. 12, 2024
Hope for lifting ban on OM, PPC chips
By The Independent
Aug. 26, 2022
Without planes, AirZim board won’t perform wonders
By The Independent
Aug. 5, 2022
Power crisis needs urgent attention
By The Independent
Jul. 29, 2022
Don’t print cash for projects
By The Independent
Jul. 22, 2022
Exploring the vibrant world of sports betting in Ethiopia
While the allure of sports betting is undeniable, it's crucial to approach it with caution and responsibility.
By Theindependent
Mar. 11, 2024
Satewave churns out power solutions for Zim
Satewave Technologies director Xiao Feng said the company has several solar solutions to address the current power challenges.
By Staff Writer
Aug. 15, 2023
Liquid Tech to increase tariffs by 50%
By Staff Writer
Mar. 31, 2023
Jotter: Students develop an integrated learning app
By Staff Writer
Mar. 17, 2023
Innovative crowd-investing app ‘PiggyBankAdvisor’ launched
By Staff Writer
Mar. 17, 2023
Meta gives up on NFTs for Facebook and Instagram
By The Verge
Mar. 15, 2023
Reasons To Buy Bitcoin From A Trading Platform
Another fundamental reason behind getting the coins from this particular space is that it provides
By Theindependent
Mar. 2, 2023
Why do banks not want people to rely upon cryptocurrencies?
Cryptocurrency transaction volume is much less than the fiat currencies, leading to a lack of liquidity in the market.
By Theindependent
Feb. 9, 2023
De Souza banks on speed, agility.

Zimbabwe U20 rugby team head coach, Shaun De Souza is happy with the team’s preparations and looking forward to their tournament opener against Tunisia.
By Austin Karonga
Apr. 19, 2024
By Austin Karonga
Mar. 28, 2024
By Kevin Mapasure
Mar. 28, 2024
By Munyaradzi Madzokere
Mar. 22, 2024
Book Review: African decolonisation in Southern Rhodesian Politics, 1950–1963
By Anotida Chikumbu
Apr. 12, 2024
Moozy captivates audience at homecoming showcase
By Khumbulani Muleya
Apr. 12, 2024
Forbes 30 Under 30 Summit Africa spotlights Zim vegan cuisine

According to forbes.com, featured speakers will include government officials, venture capitalists, CEOs and celebrities.
By Khumbulani Muleya
Apr. 5, 2024
Women take over the stage at Sofar
By Staff Writer
Mar. 28, 2024
Japanese pop culture comes to life in Harare
By Khumbulani Muleya
Mar. 22, 2024
Fawezi wraps up GBV prevention initiative
By Khumbulani Muleya
Mar. 15, 2024
New children’s book a magical adventure
By Khumbulani Muleya
Mar. 15, 2024
Herbicides: Bad news for local food security
By The Independent
May. 27, 2022
Dumpsite: Gweru feels the heat
By The Independent
May. 13, 2022
Zim to pay 100% of international hunting revenue to communities
By The Independent
Jun. 10, 2022
.
Videos
Pamela Marwisa In Conversation With Trevor
By The NewsDay
Feb. 28, 2024
Job Sikhala, Zimbabwean Opposition Politician In Conversation With Trevor
By The NewsDay
Feb. 28, 2024
ExtremeWeather: Parts of Harare experienced flash floods on Sunday
By The NewsDay
Dec. 21, 2023
Harare motorists negotiate the city’s treacherous roads
By The NewsDay
Dec. 21, 2023
Solomon Guramatunhu Day 1
By The NewsDay
Dec. 14, 2023
Sengezo Tshabangu - In Conversation With Trevor
By The NewsDay
Dec. 5, 2023
Welcome to Alpha Media Holdings Zimbabwe - NewsDay - The Standard - The Zim Independent
By The NewsDay
Dec. 5, 2023
Dock sheep tail to maintain weight

The most common way of docking tails is by using an elastic and expandable latex ring. The rubber ring is expanded with an elastrator and put over the tail, where it is released.
By Kudakwashe Gwabanayi
Mar. 22, 2024
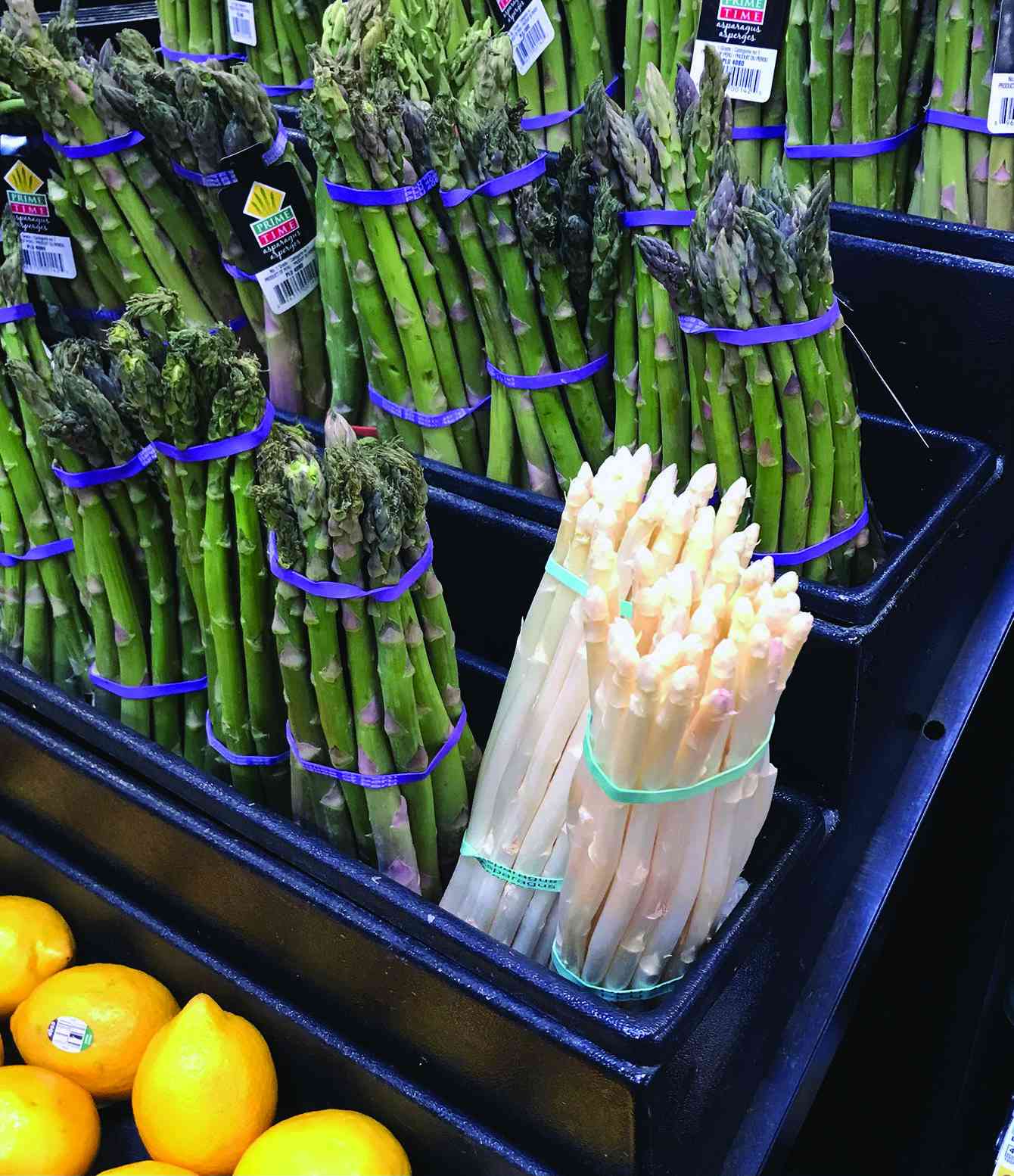
Asparagus worth your while (II)
By Kudakwashe Gwabanayi
Mar. 1, 2024
Why it makes sense to farm meat goats
By Shane Brody
Jul. 7, 2023
How to start a fish farming business
By Kudakwashe Gwabanayi
May. 26, 2023
Climate change is real, be alert
By Kudakwashe Gwabanayi
May. 12, 2023
Mahachi pays tribute to late SA gospel icon
Mahachi and Ncwane collaborated on a 2015 hit single titled Ndinoda Jesu/Ngiyamuthanda uJesu, which marked the beginning of their connection.
By Style Reporter
9h ago
Zinest calls for economic strengthening in drug abuse fight
Mazuruse said the challenging economic environment had not helped matters with limited opportunities pushing promising young minds into unbecoming behaviour.
By Style Reporter
12h ago
Health Talk : Housing, health delivery very critical components that need to be addressed
By Dr Johannes Marisa
Apr. 21, 2024
Was it witchcraft or sleep paralysis?
By Onie Ndoro
Apr. 21, 2024
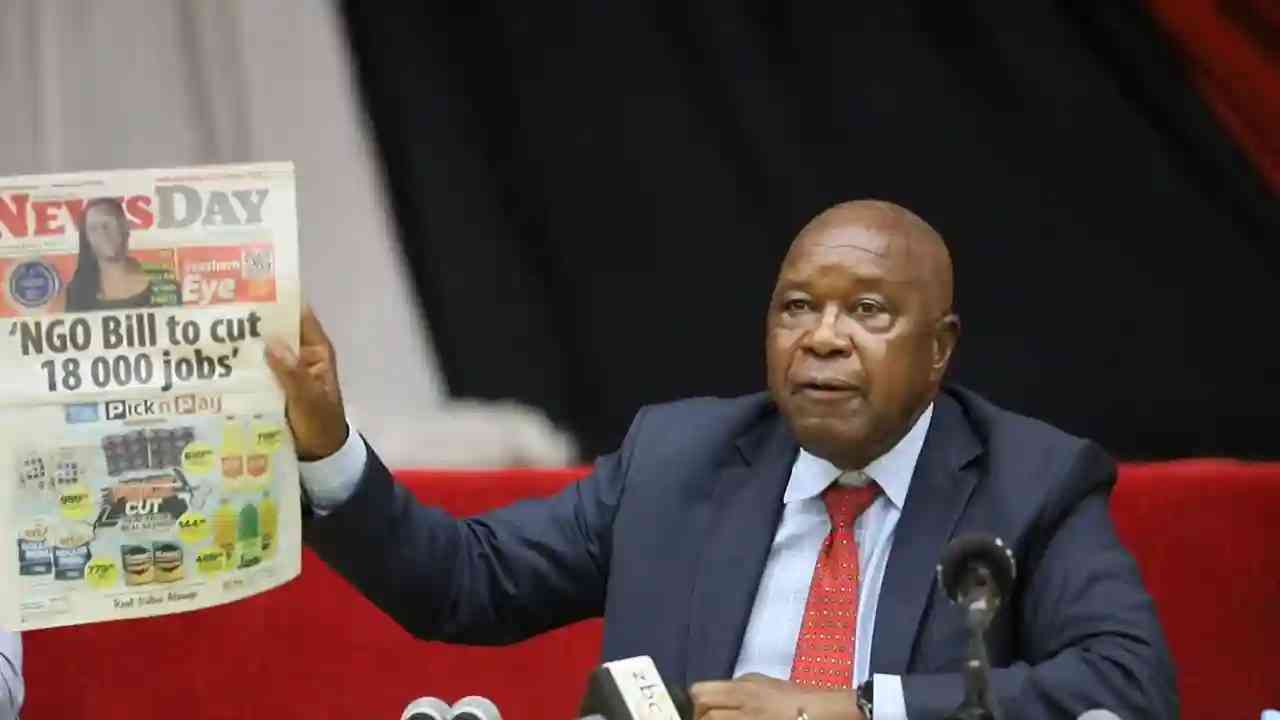
Chiwenga gives voters chilling warning
By Miriam Mangwaya
Apr. 21, 2024
Govt distributes ‘rotten’ maize in Hwange
They also revealed that the situation in the drought-hit district had become dire, pleading with the government to assist them until the next harvest.
By Blessed Ndlovu
19h ago
We’ve no capacity to deal with hunger: Chiefs
The traditional leader recently organised the Chief Dakamela Awards Ceremony in Nkayi to celebrate and recognise locals who have done well in uplifting the district.
By Silas Nkala
19h ago
Vendors battle for space at ZITF grounds
By Daniel Moyo
Apr. 22, 2024
Matabeleland concerned over army recruitment
By Silas Nkala
Apr. 22, 2024
Byo welcomes road rehabilitation projects
By Innocent Magondo
Apr. 22, 2024
China’s Coercive Expansionism a Threat to Bhutanese Sovereignty
China’s coercive expansionism poses a grave threat to Bhutanese sovereignty and regional stability.
By Khabarhub
6h ago